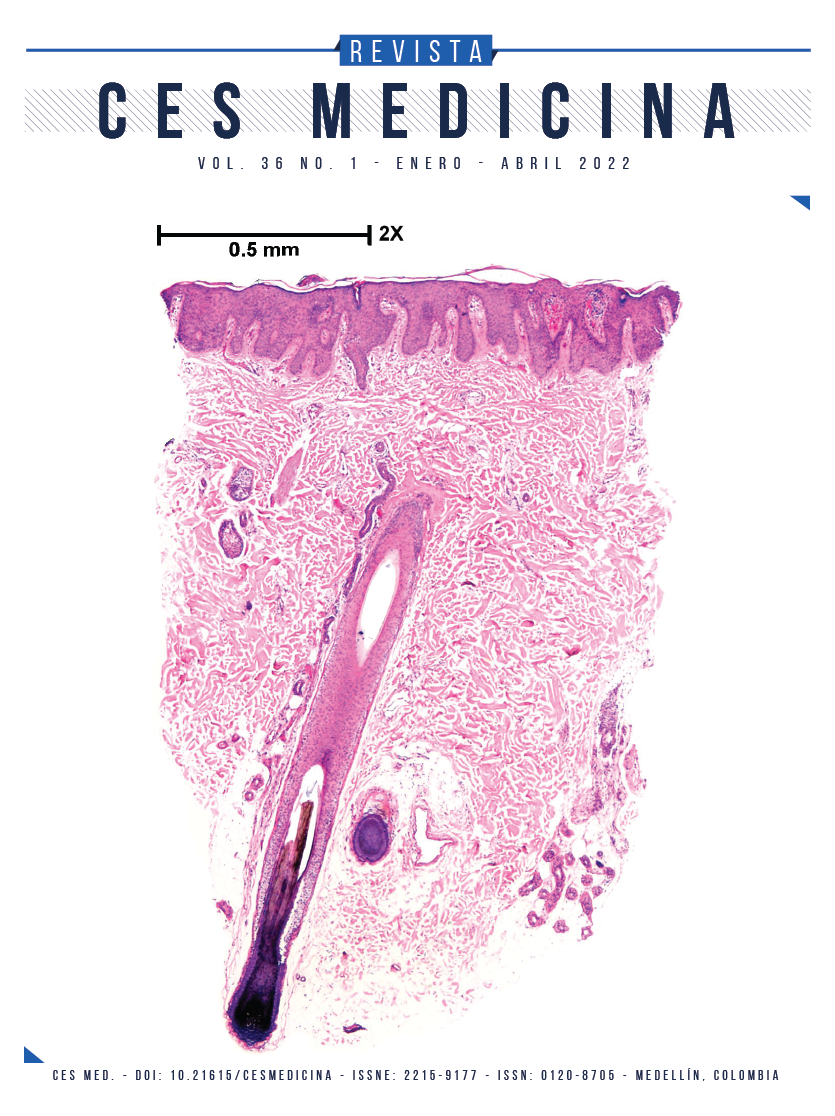
Mucocutaneous manifestations in patients hospitalized with covid-19 in a high complexity hospital
DOI:
https://doi.org/10.21615/cesmedicina.6427Keywords:
COVID-19, mucocutaneous, severity, hospitalizationAbstract
Introduction: SARS-CoV-2 is a single-stranded RNA virus that affects different organs, including the skin. Patients with this virus can present different mucocutaneous manifestations. Objective: to determine the prevalence of skin lesions in patients hospitalized for SARS-CoV-2 / COVID 19 infection at the Hospital San Vicente Fundación Rionegro between April and June 2021. Materials and methods: descriptive cross-sectional study in hospitalized patients with a diagnosis of infection by COVID-19 confirmed by serological tests and with mucocutaneous lesions. Results: of 600 patients hospitalized for COVID-19, 16 presented mucocutaneous lesions for a prevalence of 2,6 %, and among these, 13 required management in the intensive care unit due to severe acute respiratory distress syndrome or severe illness (81,25%) associated with elevated markers of poor prognosis. The most increased were PCR, LDH and/or lymphopenia. Vascular lesions were the most frequent (42,9%), manifested as purples, vasculitis, livedo racemosa, perniosis and pseudoperniosis. The eruptions or rashes were maculopapular (28.6%), erythematous (19%) and urticarial (9,5%), and ulcers in the oral cavity (8,8%) and vesicles (2,9%). 75% of these patients had skin lesions in the active phase of the disease and 25% in the resolution phase. The most frequent morbidity was arterial hypertension (30%) and diabetes (20%). six patients (37,5%) died. Conclusions: the mucocutaneous manifestations associated with COVID-19, especially those of a vascular type such as purples, vasculitis and livedo racemosa, are associated with severe forms of the disease, especially in patients with assisted mechanical ventilation with a high mortality rate.
Downloads
References
Catalá Gonzalo A, Galván Casas C. COVID-19 y piel. Actas Dermosifiliogr 2020; 111(6):447-449. doi: 10.1016/j.ad.2020.04.007.
Drenovska, K., Schmidt E, Vassileva S. Covid-19 pandemic and the skin. Int J Dermatol 2020; 59(11):1312-1319. doi: 10.1111/ijd.15189. 59:1312-1319.
Sachdevaa M., Gianottib R., Shaha, M., et al. Cutaneous manifestations of COVID-19: Report of three cases and a review of literature. J of Dermatol Sci. 2020; 98(2):75-81. doi: 10.1016/j.jdermsci.2020.04.011. 2020:75-81.
Zhao, Q., Fang, X., Pang, Z., et al. COVID-19 and cutaneous manifestations: A systematic review. J Eur Acad Dermatol Venereol. 2020; 34(11):2505-2510. doi: 10.1111/jdv.16778.
Seirafianpour F., Sodagar S., Pour A, Panahi P, Mozafarpoor M, Almasi S, et al. Cutaneous manifestations and considerations in COVID-19 pandemic: A systematic review. Dermatol Ther. 2020 Nov; 33(6):1-22. doi: 10.1111/dth.13986
Garduño-Soto M, Choreño-Parra J, Cazarin-Barrientos J. Dermatological Aspects of SARS-CoV-2 infection: mechanisms and manifestations. Arch Dermatol 2021; 313(8):611-622. doi: 10.1007/s00403-020-02156-0.
Criado P, Martínez B, Carvalho I, Van Blarcum C, Cacciolari G, Campos I. Are the cutaneous manifestations during or due to SARS‐CoV‐2 infection/COVID‐19 frequent or not? Revision of possible pathophysiologic mechanisms. Inflammation Research 2020; 69: 745-756. doi: 10.1007/s00011-020-01370-w.
Young S, Fernandez A. Skin manifestations of COVID-19. Cleve Clin J Med 2020; 183(1):1-4. doi: 10.3949/ccjm. 87a.ccc031.
Daneshgaran G, Dubin D, Gould D. Cutaneous Manifestations of COVID‐19: An Evidence‐Based Review. Am J Clin Dermatol 2020; 21(5): 627-639.doi: 10.1007/s40257-020-00558-4.
Rekhtman S, Tannenbaum R, Strunk A, Birabaharan M, Wrigte S, Grbic N, et al. Eruptions and related clinical course among 296 hospitalized adults with confirmed COVID-19. J Am Acad Dermatol 2021; 84(4):946-952. doi: 10.1016/j.jaad.2020.12.046.
Gisondi P, Plaserico S, Bordin C. Cutaneous manifestations of SARS-CoV-2 infection: A clinical update. JEADV 2020; 34(11):2499-2504. doi: 10.1111/jdv.16774.
Wollina U, Karadağ AS, Rowland-Payne C, Chiriac A, Lotti T. Cutaneous signs in COVID-19 patients: a review. Dermatol Ther 2020;33(5):1-6. doi: 10.1111/dth.13549.
Gottlieb M, Long B. Dermatologic manifestations, and complications of COVID-19. Am J Emerg Med 2020; 38(9):1715-1721. doi: 10.1016/j.ajem.2020.06.011.
Bouaziz JD, Duong TA, Jachiet M, Velter C, Lestang P, Cassius C, et al. Vascular skin symptoms in COVID‐19: a French observational study. JEADV 2020; 34(9):451-452. doi: 10.1111/jdv.16544.
Colmenero I, Santonja C, Riano M, Noguera L, Hernández A, Andina D, et al. SARS-CoV-2 endothelial infection causes COVID-19 chilblains: histopathological, immunohistochemical and ultrastructural study of seven pediatric cases. Br J Dermatol 2020; 183(4):729-737. doi: 10.1111/bjd.19327.
Iba T, Connors JM, Levy J. The coagulopathy, endotheliopathy, and vasculitis of COVID-19. Inflammation Research 2020; 69:1181–1189.
Jiménez J, Ortega D, Perosanz P, Burgos P, Vañó S, Fernández M, et al. Enanthem in Patients with COVID-19 and Skin Rash. JAMA Dermatology 2020; 156(10):1134-1136. doi: 10.1001/jamadermatol.2020.2550.
Recalcati S. Cutaneous manifestation in Covid-19: A first perspective. JEADV 2020; 34(5):212-213. doi: 10.1111/jdv.16387.
Galván C, Català A, Carretero G, Rodríguez P, Fernández D, Rodríguez A, et al. Classification of the cutaneous manifestations of COVID-19: a rapid prospective nationwide consensus study in Spain with 375 cases. Br J Dermatol 2020; 183(1):71-77. doi: 10.1111/bjd.19163.
Algaadi S. Urticaria and COVID-19: A review. Dermatol Ther 2020; 33(6):1-7. doi: 10.1111/dth.14290.
Fernández D, Ortega D, Jiménez J, Burgos P, Perosanz D, Suarez A, et al. Clinical and histological characterization of vesicular COVID-19 rashes: a prospective study in a tertiary care hospital. Clin Exp Dermatol 2020; 45(7):872-875. doi: 10.1111/ced.14277.
Martin Carreras C, Amaro Sánchez J, Lopez-Sanchez AF, Jané-Salas E, Somacarrera M. Oral vesiculobullous lesions associated with SARS-CoV-2 infection. Oral Dis 2021; 27(3):710-712. doi: 10.1111/odi.13382.
Andina D, Belloni-Fortina A, Bodemer C, Bonifazi E, Chiriac A, Colmero I. et al. Skin manifestations of COVID-19 in children: Part 1. Clinical and Experimental Dermatology 2021: 46; 444–450
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 CES Medicina

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Derechos de reproducción (copyright)
Cada manuscrito se acompañará de una declaración en la que se especifique que los materiales son inéditos, que no han sido publicados anteriormente en formato impreso o electrónico y que no se presentarán a ningún otro medio antes de conocer la decisión de la revista. En todo caso, cualquier publicación anterior, sea en forma impresa o electrónica, deberá darse a conocer a la redacción por escrito.
Plagios, duplicaciones totales o parciales, traduccones del original a otro idioma son de responsabilidad exclusiva de los autores el envío.
Los autores adjuntarán una declaración firmada indicando que, si el manuscrito se acepta para su publicación, los derechos de reproducción son propiedad exclusiva de la Revista CES Medicina.
Se solicita a los autores que proporcionen la información completa acerca de cualquier beca o subvención recibida de una entidad comercial u otro grupo con intereses privados, u otro organismo, para costear parcial o totalmente el trabajo en que se basa el artículo.
Los autores tienen la responsabilidad de obtener los permisos necesarios para reproducir cualquier material protegido por derechos de reproducción. El manuscrito se acompañará de la carta original que otorgue ese permiso y en ella debe especificarse con exactitud el número del cuadro o figura o el texto exacto que se citará y cómo se usará, así como la referencia bibliográfica completa.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |