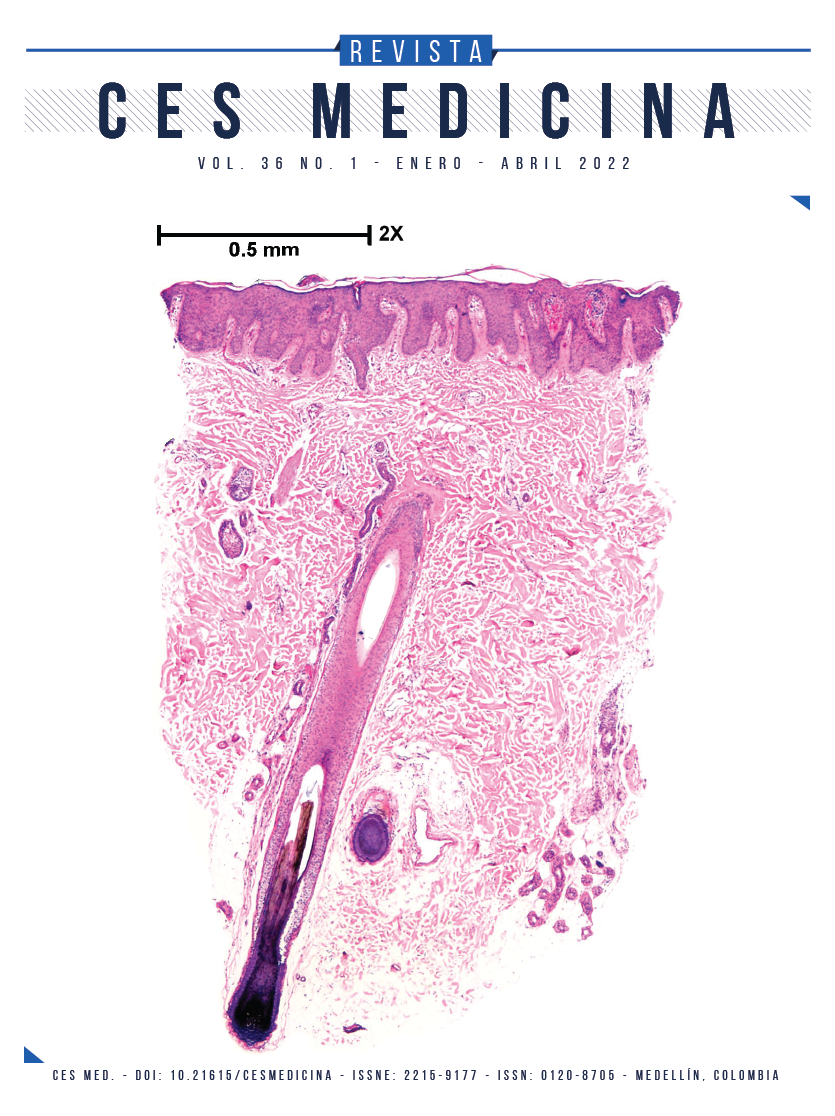
Clinical, sociodemographic, pharmacological and quality of life characterization of patients with a diagnosis of moderate to severe psoriasis treated in a specialized psoriasis clinic
DOI:
https://doi.org/10.21615/cesmedicina.6335Keywords:
psoriasis, population characteristics, quality of life, phenotype, drug therapy, heart disease risk factors, Colombia, epidemiologyAbstract
Introduction: psoriasis is a systemic, inflammatory, and chronic disease with a global prevalence between 0.6-6.5 %. It is related to multiple comorbidities and generates a significant decrease in quality of life. Objective: to characterize sociodemographic, clinical, pharmacological, and quality of life variables in a population of patients with moderate-severe psoriasis. Methods: descriptive observational study the patients with a diagnosis of severe-moderate psoriasis treated in the Clínica Integral de Psoriasis-CLIPSO between May 2018 - June 2020. A collection format was designed for defined variables and a univariate analysis was performed. Results: 948 patients were identified with a median age of 50 years (IQR: 38-60) of which 51.0 % were women. 23.6 % were incidents with a median treatment time of 114 days (IQR: 98-127) and 73.9 % were prevalent with a median treatment time of 228 days (IQR: 160-371). The type of therapy used was mainly non-biological systemic and 90.9 % of the patients were adherent to the treatment. The clinical variables were similar for both groups and the most common phenotype was psoriasis vulgaris (57.1 %). The health-related quality of life in both groups was greater than 60 points and the affected dimensions were physical and psychological health. 27.3 % of the patients had comorbidities associated with cardiovascular risk and 44.7 % were overweight. Conclusion: knowing the sociodemographic, clinical, pharmacological, and quality of life characteristics of patients with moderate-severe psoriasis allows the identification of risk factors and comprehensive management of the disease.
Downloads
References
Armstrong AW, Read C. Pathophysiology, Clinical Presentation, and Treatment of Psoriasis: A Review. JAMA - J Am Med Assoc. 2020;323(19):1945–60. https://jamanetwork.com/journals/jama/fullarticle/2766169
Hernández-Vásquez A, Molinari L, Larrea N, Ciapponi A. Psoriasis in Latin America and the Caribbean: a systematic review. J Eur Acad Dermatology Venereol. 2017;31(12):1991–8. https://pubmed.ncbi.nlm.nih.gov/28608530/
Ortega-Hernández Á, Restrepo-López N, Rosero YS, Úsuga-Úsuga F, Correa-Londoño LA, Marín-Agudelo ND, et al. Características epidemiológicas, clínicas e histopatológicas de pacientes con psoriasis y factores asociados con las formas vulgar y pustulosa. Dermatología Rev Mex. 2018;62(3):193–205.
Egeberg A, See K, Garrelts A, Burge R. Epidemiology of psoriasis in hard-to-treat body locations: Data from the Danish skin cohort. BMC Dermatol. 2020;20(1):1–8. https://doi.org/10.1186/s12895-020-00099-7
Gudjonsson JE, Elder JT. Psoriasis: epidemiology. Clin Dermatol. 2007;25(6):535–46. https://pubmed.ncbi.nlm.nih.gov/18021890/
Kowalewska B, Cybulski M, Jankowiak B, Krajewska-Kułak E. Acceptance of Illness, Satisfaction with life, sense of stigmatization, and quality of life among people with Psoriasis: A Cross-Sectional Study. Dermatol Ther (Heidelb). 2020;10(3):413–30. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC7211781/
Bhosle MJ, Kulkarni A, Feldman SR, Balkrishnan R. Quality of life in patients with psoriasis. Health Qual Life Outcomes. 2006;4:35. https://pubmed.ncbi.nlm.nih.gov/16756666/
Grupo de Trabajo de Psoriasis de la AEDV (GPs). Indices de medición de psoriasis [Internet]. https://aedv.es/wp-content/uploads/2016/07/Indices-de-medición-de-psoriasis.pdf
Rich P, Scher RK. Nail Psoriasis Severity Index: A useful tool for evaluation of nail psoriasis. J Am Acad Dermatol. 2003;49(2):206–12. https://pubmed.ncbi.nlm.nih.gov/12894066/
Cassell SE, Bieber JD, Rich P, Tutuncu ZN, Lee SJ, Kalunian KC, et al. The modified Nail Psoriasis Severity Index: validation of an instrument to assess psoriatic nail involvement in patients with psoriatic arthritis. J Rheumatol. 2007;34(1).
Rodríguez Chamorro MÁ, García-Jiménez E, Amariles P, Rodríguez Chamorro A, Faus MJ. Revisión de tests de medición del cumplimiento terapéutico utilizados en la práctica clínica. Aten Primaria. 2008;40(8):413–7. https://www.elsevier.es/es-revista-atencion-primaria-27-articulo-revision-tests-medicion-del-cumplimiento-13125407
World Health Organization. WHOQOL: Measuring Quality of Life [Internet]. 2012. https://www.who.int/tools/whoqol/whoqol-bref
Cardiff University. Dermatology Life Quality Index [Internet]. New York, NY: Springer New York; https://www.cardiff.ac.uk/medicine/resources/quality-of-life-questionnaires/dermatology-life-quality-index
Rachakonda TD, Schupp CW, Armstrong AW. Psoriasis prevalence among adults in the United States. J Am Acad Dermatol. 2014;70(3):512–6. https://pubmed.ncbi.nlm.nih.gov/24388724/
Schmieder A, Peitsch WK. Psoriasis in besonderen Lokalisationen. Hautarzt. 2016;67(6):454–63. https://link.springer.com/article/10.1007/s00105-016-3806-2
Castro-Ayarza JR, Casadiego EJ, Medina DC. Descripción de los pacientes con diagnóstico de psoriasis en un centro dermatológico de referencia de Bogotá, Colombia. Dermatologia Rev Mex. 2017;61(4):283–91. https://dermatologiarevistamexicana.org.mx/article/descripcion-de-los-pacientes-con-diagnostico-de-psoriasis-en-un-centro-dermatologico-de-referencia-de-bogota-colombia/
Kunz M, Simon JC, Saalbach A. Psoriasis: Obesity and Fatty Acids. Front Immunol. 2019;10:1807. https://pubmed.ncbi.nlm.nih.gov/31417571/
Gelfand JM, Troxel AB, Lewis JD, Kurd SK, Shin DB, Wang X, et al. The risk of mortality in patients with psoriasis: Results from a population-based study. Arch Dermatol. 2007;143(12):1493–9. https://pubmed.ncbi.nlm.nih.gov/18086997/
Coumbe AG, Pritzker MR, Duprez DA. Cardiovascular risk and psoriasis: Beyond the traditional risk factors. Am J Med. 2014;127(1):12–8. https://pubmed.ncbi.nlm.nih.gov/19177544/
Wilson FC, Icen M, Crowson CS, McEvoy MT, Gabriel SE, Kremers HM. Incidence and clinical predictors of psoriatic arthritis in patients with psoriasis: A population-based study. Arthritis Care Res. 2009;61(2):233–9. https://pubmed.ncbi.nlm.nih.gov/19177544/
Liao W, Singh R, Lee K, ucmak derya, Brodsky M, Atanelov Z, et al. Erythrodermic psoriasis: pathophysiology and current treatment perspectives. Psoriasis Targets Ther. 2016;Volume 6:93–104. https://pubmed.ncbi.nlm.nih.gov/28856115/
Reynolds KA, Pithadia DJ, Lee EB, Wu JJ. Treatments for inverse psoriasis: a systematic review. J Dermatolog Treat. 2020;31(8):786–93. https://pubmed.ncbi.nlm.nih.gov/31100992/
Omland SH, Gniadecki R. Psoriasis inversa: A separate identity or a variant of psoriasis vulgaris? Clin Dermatol. 2015;33(4):456–61. https://pubmed.ncbi.nlm.nih.gov/26051061/
Schons KRR, Knob CF, Murussi N, Beber AAC, Neumaier W, Monticielo OA. Nail psoriasis: A review of the literature. An Bras Dermatol. 2014;89(2):312–7. https://www.ncbi.nlm.nih.gov/pmc/articles/PMC4008063/
Bardazzi F, Starace M, Bruni F, Magnano M, Piraccini BM, Alessandrini A. Nail psoriasis: An updated review and expert opinion on available treatments, including biologics. Acta Derm Venereol. 2019;99(6):516–23. https://pubmed.ncbi.nlm.nih.gov/30521057/
Lee YW, Park EJ, Kwon IH, Kim KH, Kim KJ. Impact of psoriasis on quality of life: Relationship between clinical response to therapy and change in health-related quality of life. Ann Dermatol. 2010;22(4):389–96. https://pubmed.ncbi.nlm.nih.gov/21165207/
Augustin M, Radtke MA. Quality of life in psoriasis patients. Expert Rev Pharmacoeconomics Outcomes Res. 2014;14(4):559–68. https://pubmed.ncbi.nlm.nih.gov/24820452/
Menter A, Griffiths CE. Current and future management of psoriasis. Lancet (London, England). 2007;370(9583):272–84. https://pubmed.ncbi.nlm.nih.gov/17658398/
Kim IH, West CE, Kwatra SG, Feldman SR, O’Neill JL. Comparative efficacy of biologics in psoriasis: a review. Am J Clin Dermatol. 2012;13(6):365–74. https://pubmed.ncbi.nlm.nih.gov/22967166/
Augustin M, Holland B, Dartsch D, Langenbruch A, Radtke MA. Adherence in the treatment of psoriasis: A systematic review. Dermatology. 2011;222(4):363–74. https://pubmed.ncbi.nlm.nih.gov/21757881/
Svendsen MT, Feldmann S, Tiedemann SN, Sørensen ASS, Rivas CMR, Andersen KE. Improving psoriasis patients’ adherence to topical drugs: a systematic review. J Dermatolog Treat. 2020;31(8):776–85. https://pubmed.ncbi.nlm.nih.gov/31122090/
Saeki H, Imafuku S, Abe M, Shintani Y, Onozuka D, Hagihara A, et al. Poor adherence to medication as assessed by the Morisky Medication Adherence Scale-8 and low satisfaction with treatment in 237 psoriasis patients. J Dermatol. 2015;42(4):367–72. https://pubmed.ncbi.nlm.nih.gov/25720544/
Downloads
Published
How to Cite
Issue
Section
License
Copyright (c) 2022 CES Medicina

This work is licensed under a Creative Commons Attribution-NonCommercial-ShareAlike 4.0 International License.
Derechos de reproducción (copyright)
Cada manuscrito se acompañará de una declaración en la que se especifique que los materiales son inéditos, que no han sido publicados anteriormente en formato impreso o electrónico y que no se presentarán a ningún otro medio antes de conocer la decisión de la revista. En todo caso, cualquier publicación anterior, sea en forma impresa o electrónica, deberá darse a conocer a la redacción por escrito.
Plagios, duplicaciones totales o parciales, traduccones del original a otro idioma son de responsabilidad exclusiva de los autores el envío.
Los autores adjuntarán una declaración firmada indicando que, si el manuscrito se acepta para su publicación, los derechos de reproducción son propiedad exclusiva de la Revista CES Medicina.
Se solicita a los autores que proporcionen la información completa acerca de cualquier beca o subvención recibida de una entidad comercial u otro grupo con intereses privados, u otro organismo, para costear parcial o totalmente el trabajo en que se basa el artículo.
Los autores tienen la responsabilidad de obtener los permisos necesarios para reproducir cualquier material protegido por derechos de reproducción. El manuscrito se acompañará de la carta original que otorgue ese permiso y en ella debe especificarse con exactitud el número del cuadro o figura o el texto exacto que se citará y cómo se usará, así como la referencia bibliográfica completa.
| Article metrics | |
|---|---|
| Abstract views | |
| Galley vies | |
| PDF Views | |
| HTML views | |
| Other views | |